by Andrew I Spielman
How to cite this page: Spielman, AI. History of Oral Diagnosis, Medicine, Pathology and Radiology. In: Illustrated Encyclopedia of the History of Dentistry, 2023. https://historyofdentistryandmedicine.com/
History of oral diagnosis, medicine, pathology, and radiology
Before tackling the history of oral diagnosis, medicine, pathology, and radiology, one has to define what is covered by the above terms, for they are different at different times in history, especially in the context of modern definitions. Initially, all of the above was (barely) a single discipline, with radiology being non-existent until 1895. As discoveries made it possible, specialization and separation of disciplines followed. This chapter will consider any soft and hard tissue pathology, local or systemic, with oral manifestations, visible (lesions) or invisible (plaque, salivary components, immunology, microbiology, virology, etc.). For good measure, such areas were not the domain of tooth drawers. Physicians handled them and, if surgery was involved, by surgeons or barber surgeons.
The earliest description of oral diagnosis/medicine/pathology comes from the Ebers Papyrus, written during the XVIIIth Dynasty, around 1500 BCE. It contains recipes to strengthen the teeth (periodontal condition) or for treatment of the “bennut” – “blisters in the teeth” (1). Many prescriptions included honey, onion, milk, dates, and medicinal plants. Facial swelling in the Edwin Smith Papyrus from the same period recommended placement of fresh meat on the swollen area followed by daily, topically applied grease, honey, and lint (2).

Ebers Papyrus. Compiled ~ 1550 BCE, it contains about 700 magic formulas of folk medications. Currently, it is preserved at the library of the University of Leipzig, Germany.
In Ancient India, Susruta Samhita, a first millennium BC script, had an extensive segment dedicated to treating oral diseases, including sixty-five oral conditions affecting the lips, gums, teeth, tongue, palate, throat, and the oral cavity as a whole (3).
The Corpus Hippocraticus, the body of work attributed to followers of Hippocrates and the school of Kos, contained tips for diagnosing and managing oral diseases and symptoms of local and systemic conditions. The School of Kos, in contradistinction to the School of Kneidos, just across the strait in the southeastern Aegean Sea, considered a patient holistically and provided a logical prognosis based on careful patient observation. In this regard, the Coan Prenotions published in 1525, a translation of an earlier Arabic publication, is now universally accepted to be a derivative of the Prognostics, a Hippocratic work and the earliest compilation of oral diagnosis (4). The Coan Prenotions was divided into 24 chapters with 640 prognostic statements. They covered, among others, such topics as headache, prognostics: 156–184, face and mouth, prognostics 208–239, and throat and neck prognostics, 256–272. The Corpus Hippocraticus described several forms of oral ulcers (aphthae), cold sores (herpes), the triad symptoms of what today we define as Bechet’s Syndrome (aphthae, genital ulcers, and eye inflammation), and gingivitis (ulitis) (5).
Hippocrates of Cos. Opera Omnia – Frontispiece of 1596 edition.
Such knowledge was evident in Roman times as well. For instance, Aulus Cornelius Celsus (25 BCE- 50 CE), the Roman physician and author of De Re Medicina, is the first to describe the four cardinal signs of inflammation: tumor, rubor, calor, dolor, swelling, redness, warmth and pain (6). Further, the great herbal collection of Dioscorides (40-90 C.E.) contains recipes for the treatment of bad breath, strengthening the teeth and gums (myrrh resin), and oral ulcers (pomegranate) (7).
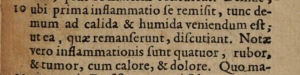
The text where Celsus describes the four cardinal signs of inflammation: “Notae vero inflammationis sunt quatuor, rubor, & tumor, cum calore, et dolore”. “There are for signs of inflammation, redness, and swelling, with heat and pain — reproduced from a 1687 edition of De Re Medicina, chapter 10, p.139.
The early Medieval Arab physicians described preparations to treat mouth abscesses in the Syriac Book of Medicine, a manuscript dated to the mid-first millennium CE. Such preparations contained juice of mulberries, grapes, honey, crocus, and myrrh (8). Avicenna’s (980-1037) Canon Medicinae, one of the most famous medical texts of all time, contained comprehensive descriptions of diseases of the mouth and tongue (9).
Regarding oral medicine/pathology topics, medieval physicians and surgeons like Guy de Chauliac, Ambroise Paré, and Fabricius ab Aquapendente usually would repeat and synthesize knowledge of Greek, Roman, and Arab physicians before them. Few original ideas are found in such works up until the 17th century. Then, a self-educated draper and part-time janitor, enthusiastic lens-crafter, the Dutch Antony van Leeuwenhoek (1632-1723), discovered the microscopic world. His invention of the microscope opened up new possibilities in understanding the unseen world of the oral cavity: oral microbes, dental plaque, and dentin structures, to name a few. Leeuwenhoek wrote 285 scientific letters to the Royal Society in London during his lifetime. His contribution earned this laic a unique membership in Society, the only non-scientist to ever do so (10).
A particularly important contribution to the advancement of oral diagnosis/medicine/pathology comes from the Swiss Albrecht von Haller (1708-1777), an erudite professor of physiology, a pupil of Hermann Boerhaave and Bernhard Siegfried Albinus at the University of Leiden. His studies on mastication, saliva, swallowing, taste, and smell were original and essential to understanding normal oral physiology (11). Similarly important is Lorenz Heister (1683-1758), a German surgeon with extensive knowledge, including cancer of the lip and mouth and management of other oral pathologies (12).

Herman Boerhaave – 1768-1738
Pierre Fauchard’s (1678-1761) two-volume work, Le Chirurgien Dentiste, covered all areas of dentistry, including oral medicine and pathology. For instance, in volume I of his work, specific sections was dedicated to gingival ulcerations, salivary stones, or epulis. However, Fauchard’s contributions did not lie either in oral medicine or oral pathology. The strength of his work was comprehensiveness, especially in restorative, periodontics, and prosthodontics (13).

A page from Pierre Fauchard’s 1746 edition of Le Chirurgiene Dentiste, depicting extraction forceps.
The 19th century saw the compilation of symptoms of systemic conditions with oral manifestations. One of the most important categories of such diseases was those dermatological conditions with oral mucosal signs and symptoms. Sir Erasmus Wilson (1809-1884), an English surgeon and dermatologist, was the first to make the connections (14) in his 1846 publication On Diseases of the Skin (15).
The first publication in America that specialized in what we would consider Dental Medicine (a precursor of Oral Medicine and Oral Pathology) was Thomas E. Bond’s 1851 work entitled: A Practical Treatise on Dental Medicine. In the introduction, he states: “The relations of the teeth and their appendages with other, and even with vital parts, are sufficiently important to be carefully studied both by the Dentist and Physician.” The statement shows general ignorance of the relationship between the oral cavity and the rest of the body (16). The text includes topics covered today by general, systemic, and oral pathology, medicine, microbiology, immunology, and oral and maxillofacial surgery.
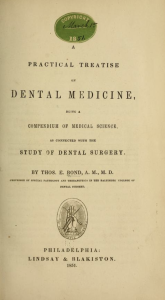
The cover of Thomas Bond’s 1851 work entitled A Practical Treatise on Dental Medicine.
Two of the important oral clinicians of the 19th century, instrumental in establishing the discipline of oral medicine and pathology was Sir John Tomes (1815-1895), an educator, founder of the Dental Hospital of London, and the first president of the British Dental Association (17), and Sir Jonathan Hutchinson (1828-1900), considered the Father of Oral Medicine. Before the field of Oral Diagnosis, Medicine, and Pathology could exist, science had to evolve in other areas of medicine. The development of microscopic anatomy by Theodor Schwann (1810-1882) and microscopic pathology by Rudolph Virchow (1821-1902), two giants of 19th-century German science, were crucial in establishing the field. Furthermore, the seminal discoveries of Ignaz Semmelweis (1846) on puerperal fever, Louis Pasteur’s defining of the microbial nature of the disease (1864), aseptic surgery promoted by Joseph Lister (1867), the Koch Postulates enunciated by Robert Koch (1884) and the chemo-parasitic theory of caries by Willoughby D Miller (1889), all contributed to the advancement of the field.

Ulcerative endocarditis of the mitral valve, an image from Rudolph Virchow’s Cellular Pathology, 1860.
Using biopsy, microscopic anatomy, and clinical diagnosis by a series of investigators during the end of the 19th and beginning of the 20th century led to identifying unique local or systemic conditions with oral manifestations. These include vitamin B2, B3, B5, B6, and B9 deficiencies (18), amyloidosis (19), leukoplakia (20), lupus erythematosus (21), aphthous stomatitis (recurrent aphthous ulcers) (22), stomatitis aphthous (23), Behçet’s Disease (24), herpetic stomatitis (25), erythema multiforme (Stevens-Johnson Syndrome) (26) and pemphigus (27), to name a few. Discoveries in apparently unrelated fields of medicine also advanced oral medicine and pathology. For instance, Alexander Fleming’s (1881-1955) accidental discovery of salivary lysozyme (28) created openings in understanding oral defense mechanisms and, decades later, the establishment of the field of salivary research (see the section on the History of Oral Biology and Oral Diagnostics).
The establishment of the field of Oral Medicine, Pathology, and Diagnosis in the 20th century could not exist without the contribution of key individuals such as Bernhard Gottlieb (1885-1950), Balint Orban (1899-1960) in oral histology at the University of Vienna, Kurt Hermann Thoma (1883-1972) at Harvard University in Oral Pathology, Martin Rushton at Guy’s Hospital and Lester W. Burket (1907-1991) at University of Pennsylvania in Oral Medicine.
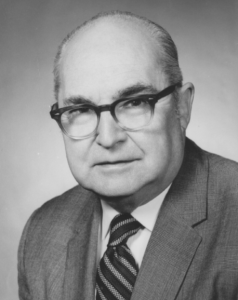
Lester W. Burket, the “Father of Oral Medicine”, professor at the University of Pennsylvania School of Dental Medicine, 1907-1991.
The field evolved, specialized, and subdivided as time passed. For instance, Francis McCarthy was first to introduce oral medicine lectures to the dental curriculum (at Tufts U.), Samuel Charles Miller of NYU helped create the Academy of Dental Medicine (now called American Academy of Oral Medicine), Irving Glickman (1914-1972), of Tufts U. established concepts and criteria for the classification of periodontal disease, Sol Silverman Jr. (1926-2014) of UCSF, was a pioneer of oral cancer, Sir David Mason (1928- ) of Glasgow University, Scotland along with Herbert Dean Millard (1924-2013) of Michigan U. created the World Workshops on Oral Medicine (now in its 7th iteration), Crispian Scully (1945-2017) of University College London and Stephen James Challacombe of King’s College (1946- ) of the UK, along with others established the European Association of Oral Medicine.
Although Oral Medicine officially was not recognized as a specialty in the US until 2020, it was unofficially established in the US in 1925s by combining dermatological and oral mucosal symptoms to manage a unique population of patients and to establish the first society in 1945. Oral pathology was established as a specialty in 1948 in the US, and soon other countries followed suit.
The history of oral radiology did not start with Wilhelm Conrad Röntgen, a German-Dutch physician’s accidental discovery of the cathode rays (X-ray) in November 1895 (29). Before Roentgen, Sir William Morgan and Michael Faraday generated X-rays in 1795 and 1800, respectively (29). Not knowing the source of the radiation, Röntgen called it X-rays. Alpha, beta, and gamma rays were discovered in 1900 and 1903. Within two weeks after Röntgen’s December 31, 1895 publication, Otto Walkhoff, a German dentist, took the first dental X-ray (30), followed by a few more weeks by Dr. Frank Harrison of Sheffield, UK. Harrison presented his experience at a meeting of the British Medical Association in January 1896 (31). By February 1896, Walter König, a Frankfurt physician, was also using X-rays in clinical diagnosis of fractures and dentistry. The first X-ray machines used in the UK or Germany required dental patients to be exposed for 25-30 minutes, but Harrison developed quicker exposure techniques within a few months (32). To reduce the gagging reflex, topical application of cocaine was advocated. Walkhoff and his colleague Fritz Giesel were the first to establish a dental X-ray laboratory in 1896 (30). The first to use in the US was C. Edmund Kells Jr. (1856-1928) in April or May 1896. Kells improved the technique by using a parallel positioning of the film, adding a film holder and a board to protect the face from the scatter.

Taking a dental X-ray at New York College of Dentistry in 1903. Exposure to X-ray was ~20 minutes. Photo from the Archives of NYU College of Dentistry. Reproduced with permission.
By 1896 the first textbook on X-rays was published. William James Morton, the son of William T.G Morton, the discoverer of ether anesthesia, was instrumental in publicizing its use in dentistry, co-authoring a book, and making presentations and public demonstrations at scientific meetings (33, 34). A key contributor to improving the detection and recording of the X-ray image comes from Thomas Edison of Menlo Park, NJ, whose lab created sensitive fluorescent screens and established the fluoroscopy method (34).
Teaching dental radiology was not far behind. The first course in dental radiology was established in 1909 at Indiana Dental College (today Indiana University School of Dentistry) by Howard R. Raper, the first to practice as a specialist in dental radiology. Radiology, though, occupied a relatively minor role in dental curricula in the early years. In 1920, for instance, the clinical radiology curriculum, approved by the Dental Educational Council, represented 1.1% or 16 hours of the 1424-hour clinical curriculum (35).
The side effects of the dental X-rays were evident almost as soon as they started to be used. Frank Harrison’s assistant developed irritation of the face exposed to lengthy radiation during the first 8 months of use in 1896. In the US, Charles E. Kells Jr.’s constant exposure to X-rays led to a series of amputations, starting with his left hand and ending with the entire left arm in 1926. Eventually, Kells committed suicide in 1928. In the US, William Herbert Rollins, a Boston dentist, introduced steps to protect patients and providers from the harmful effects of radiation. He instituted leaded housing for the X-ray source and collimators and was among the first to link radiation to its side effects (36). Guidelines for protection were not far behind. In 1915, 20 years after its introduction, the British X-ray Radium Protection Committee finally issued its guidelines. Seven years later, in 1922, the American Roentgen Ray Society issued similar provisions. Radiation exposure at the time could be as high as 7500 mSv/year. One hundred years later, the exposure limit will not exceed 20 mSv/year.

Charles Edmund Kells Jr., the Father of American Dental Radiology, a graduate of New York College of Dentistry, was the first to use dental radiography in the US.
Technology has continuously improved X-ray radiograph source, focus, and efficiency. By 1913 William David Coolidge (1873-1975), an American engineer and physical chemist, invented a smaller, more manageable X-ray tube source using a tungsten filament, the Coolidge Hot Cathode Tube. It was adjustable to provide a controlled amount of X-rays. That same discovery led to the invention of the incandescent lamp bulb. The types of dental radiographs taken were primarily periapical and occlusal. In 1925 Howard R. Raper suggested to Eastman Kodak to introduce the bitewing radiograph to detect interproximal caries. Raper is also credited with the bisecting-angle technique.
As X-rays machine shrunk and became safer, their use was widely adopted. By the 1940-50s, X-ray units were either wall mounted in the dental office or attached to the dental chair.
Similar to the machines, the X-ray films consistently improved. Since 1919, when a cellulose nitrate hand-wrapped film was used, the speed of the film doubled every 20 years until 1955, when the D-film was introduced at 8-20 times higher speed. Higher speed meant shorter exposure. By 1981 the E-speed film followed, and in 2000, the F-speed was introduced, further reducing exposure time. In approximately 100 years, the field moved from 1500-second exposure (25 minutes) to 1-2 seconds today (30).
The history of panoramic radiography essentially started in Scandinavia. Although the inventions of Alvin F. Zulauf from the US, Hisatugu Numata from Japan, and K. Heckmann from German helped his work, it was Yrjö V. Paatero (1901-1963) of Finland who gets most of the credit for his 1946 publication (37) that set the stage for widespread commercial application and clinical use of the panoramic X-ray. Paatero initially used a fixed X-ray source and a curved intraoral film. Soon, he placed the film extra-orally in front of the patient and moved the X-ray source in a semicircular fashion to create the panoramic image (38).
Computers revolutionized radiology as well. Computed Tomography (CT) and digital radiography were introduced in the 1980s and 1990, respectively. The transition from film to digital is still ongoing, but data from Sweden, for instance, shows a 98% conversion among Swedish dentists (39).
Other types of radiographs used in dentistry include cephalometric radiographs, introduced after World War II, and computerized cephalometrics, introduced in the late 1960s. Sialography and contrast radiographs of salivary glands were used from 1925 but were replaced by CT, MRI, and ultrasound techniques (30). Dental Tomography was first experimented with in the 1930s and gradually improved in the following decades. A helical motion of the tomographic unit (helical tomography) was introduced in 1988, but with the invention of cone-beam computed tomography (CBCT), a 3D imaging technique replaced it by the late 1990s. CBCT is now used almost exclusively for most hard tissue visualization, including for implant placements.
An infamous phase of oral pathology and oral surgery was at the beginning of the 20th century when William Hunter, an English physician, single-handedly promoted the idea of “oral sepsis” caused by staphylococcus and streptococcus pyogeneus harbored in the oral cavity.40 Through a series of articles starting in 1900 (Lancet, Dental Reporter, Br. Dent. J.), Hunter denounced the incompetence of the dental profession in covering up such sources of focal infection that led to systemic conditions. In the most publicized speech at the opening of the McGill Medical School in 1911, Hunter reiterated his position of the need to get rid of these infections, resulting in unnecessary extractions41,42 He stated ’Gold fillings. gold caps, gold bridges, gold crowns, fixed dentures, built in, on, and around diseased teeth, form a veritable mausoleum of gold over a mass of sepsis to which there is no parallel in the whole realm of medicine or surgery”.

Hunter denounced the dental profession in this 1900, Lancet article accusing it of incompetence.
The Oral Sepsis theory led to the removal of countless teeth. In 1912, this was replaced by the Focal Infection theory proposed by Frank Billings.43 By 1938, William and Burkett declared that “there is no good scientific evidence to support the theory”.44,45
- Shklar, Chernin p.23
- ibid p.27
- ibid p.36
- Hippocrates
- Askitopoulou
- Celsus p.139
- Shklar, Chernin p.111
- ibid p.163
- ibid p.183
- Leeuwenhoek
- von Haller p.279-294
- Shklar, Chernin p.412-19
- Fauchard vol I p.182, p.236
- Cooke
- Wilson
- Bond
- Tomes
- Afonsky; Shklar and Chernin p.718
- Selikoff and Robitzek
- McCarthy
- Monash
- Sibley
- Mikulitz and Kummel
- Behçet
- Rogers et al.
- Stevens, Johnson
- Lever, Talbott
- Fleming
- Pauwels, Röntgen
- Pauwels p. 238
- Harrison
- Bird
- Morton and Hammer
- Morton p.484
- Gies p.121
- Rollins
- Paatero, Tammisalo
- Hallikainen
- Svenson
- Hunter (a)
- Hunter (b)
- Hunter (c)
- Billings
- Williams and Burkett
- JADA Editorial
References and notes on oral diagnosis, medicine, pathology, and radiology
Afinsky, Dimitry (1955). Oral lesions in Niacin, Riboflavin, Pyridoxin, Folic Acid, and Panthotenic Acid deficiencies in Adult dog. Oral Surg, Oral Med, Oral Path, 8:207-212.
Askitopoulou, Helen, Nyktari, Vasileia, Papaioannou, Alexandra et al. (2017). The origins of oral medicine in the Hippocratic collected works. J. Oral Med Path. 46:689-694.
Behçet H. (1937). Über rezidivierende, Aphhöse, durch ein Virus verursachte Geschwüre am Munde, am Auge und an Genitalien. Dermatol. Wochenschr. 105:1152–1157.
Billings, Frank. (1911). Chronic focal infections and their etiologic relations to arthritis and nephritis. Arch Intern Med (Chic). 1912;IX(4):484-498. doi:10.1001/archinte.1912.00060160087007, https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/653275
Bird, Peter D (1981). The development of dental radiology. Brit. Dent. J. 151:28-31.
Bond, Thomas Emerson (1851). A practical treatise on dental medicine as connected with the study of dental surgery. Lindsey and Blakiston, Philadelphia. (first oral medicine and pathology text). https://www.google.com/books/edition/A_Practical_Treatise_on_Dental_Medicine/ztEvAQAAMAAJ?hl=en
Celsus, Cornelius Aurelius (1688). De Medicina Libri Octo, Apud Joannem Wolters, Amstelædami, Chapter X, pp. 139, §10. (Notæ vero inflammationis sunt quatuor, rubor & tumor, cum calore et dolore – Signs of inflammation are four, redness and swelling with heat and pain. (signs of inflammation).
Cooke, Brian E.D. (1981). History of Oral Medicine. Brit. Dent J. 151:11-13. (Erasmus Wilson, dermatologist connected systemic and oral symptoms in Oral Medicine).
Fauchard, Pierre (1746). Le Chirurgien Dentiste p.182 (salivary stone), p.236 (epoulis). Paris.
Fleming, Alexander (1922). On a remarkable bacteriolytic element found in tissues and secretions, Proceedings of the Royal Society, B93: p.306-317.
Gies, William J. (1926). Dental Education in the United States and Canada: A report of the Carnegie Foundation for the Advancement of Teaching. New York, p.120-121.
Hallikainen, Dorrit (1996). History of Panoramic Radiography. Acta Radiologica, 37:3, 441-445. https://doi.org/10.3109/02841859609177678
Harrison, Frederick (1896). The New Photography and its Application to Dental Practice. J Br Dent Assoc 17:343-344.
Hippocrates of Kos (1576). Magni Hippocratis Coaca Præsagia (Translated and edited by Jacques Houllier. Published in Lyon, 1576 by Guillaume Rouille).
Hunter WD. (1900a). Oral sepsis as a cause of disease. Br Med J. 2:215–216.
Hunter WD (1911b). The role of oral sepsis and of antisepsis in medicine. Lancet, 1:79–86.
Hunter WD (1911c). The role of sepsis and antisepsis in medicine and the importance of oral sepsis as its chief cause. Dent Register, 65:577–611.
JADA Editorial (1951) – Summaries of opinions about importance of focal infection in systemic disease. 1951, 42:694-697.
Leeuwenhoek, Antony van (2020). Lens on Leeuwenhoek. https://lensonleeuwenhoek.net/content/letters (accessed June 21, 2020).
Lever Walter F, Talbott John H (1942). A clinical analysis and follow-up study of sixty-two patients. Arch. Dermatol. Syphilol. 46:348-357.
McCarthy, Francis (1936). Etiology, pathology and treatment of leukoplakia buccalis. Arch Dermatol. 34:612-621.
Mikulitz J and Kummel W (1898). Krankheiten des Mundes (Diseases of the Mouth). Chapter 66. Gustav Fisher, Jena.
Monash, Samuel (1931). Oral Lesions of Lupus EWrythematosus. Dental Cosmo0s 73:511-515.
Rogers, Arthur M, Coriell Lewis L, Blank Harvey, McNair Scott Thomas F (1949). Acute herpetic gingivostomatitis in the adult. New England J Med. 241:330-333.
Morton, William J and Hammer Edwin W. (1896). The X-Ray or Photography of the Invisible and its Value in Surgery. American Technical Book Co. New York, pp. 196.
Morton, William James (1896). The X-Ray in Dentistry. Dental Cosmos, 38(6): 478-486. (describing Edison’s fluorescent screen for capturing X-rays.)
Paatero, Yrjö V. (1946). Sunnittelemastani uudesta hampaiden rontgenkuvaustekniikasta. Suomen Hammasla Wriseuran Toimituksia 86: 37. (English summary: A new radiographic method in dentistry.)
Pauwels, Ruben (2020). History of Dental Radiography: Evolution of 2D and 3D Imaging Modalities. Medical Physics International. Special Issue. History of Medical Physics. 3:235-277. (Excellent review of the history of dental radiology).
Rollins, William Herbert (1901). X-light kills. Boston Medical and Surgical Journal. 144:173-
Röntgen, William (1895). Uber eine neue Art von Strahlen. Vorläufige Mitteilung. Aus den Sitzungsverichten der Würzburg Physic. -medic. Gesellschaft Würzburg: 137-147.
Selikoff, Irving, J and Robitzek, Edward H (1947). Gingival biopsy for the diagnosis of generalized amyloidosis. Am. J. Pathol. 23:1099-1108.
Shklar, Gerald and Chernin, David (2001). A sourcebook of dental medicine. Maro Publications, Waban, MA, p.23 (Ebers Papyrus); Edwin Smith Papyrus (p.27); Susruta Samhita, India (p.36); Dioscorides p.111, Arab medicine p.163. Lorenz Heister p.412-19; Vitamin B deficiencies – p.718
Sibley, W.K. (1899). Neurotic ulcers of the mouth. Brit. Med. J. 1:900-906.
Stevens, A.M. and Johnson, F.C. (1922). A new eruptive fever associated with stomatitis and ophthalmia. Report of two cases in children. Am. J Dis. Child. 24:526-531.
Svenson, B., Ståhlnacke, K., Karlsson, R., Fält, A. (2017). Dentists’ use of digital radiographic techniques: Part I – intraoral X-ray: a questionnaire study of Swedish, Acta Odontol Scand, 2018 Mar;76(2):111-118. doi: 10.1080/00016357.2017.1387930. Epub 2017 Oct 11.
Tammisalo, Erkki H. (1975). Professor Yrjö V. Paatero – The Pioneer of Panoramic Oral Tomography. Dento Maxillofacial Radiology 4(1):53-56. https://doi.org/10.1259/dmfr.1975.0010
Tomes, John Sir (1859). A System of Dentistry. London.
von Haller, Albrecht (1751). Primae Linae Physiologiae in Usum Praelectionum Academicarum p.279-294.
Williams NB, Burkett LW. Focal infection – a review. Philadelphia Med 1951:46,1509; (End of the Focal infection theory).
Wilson, Erasmus (Sir) (1847). On Diseases of the Skin. Lea and Blanchard, Philadelphia, pp.447 https://www.google.com/books/edition/_/qTlHAQAAMAAJ?hl=en&gbpv=1
2023 © Copyright HistoryofDentistryandMedicine.com
